Description
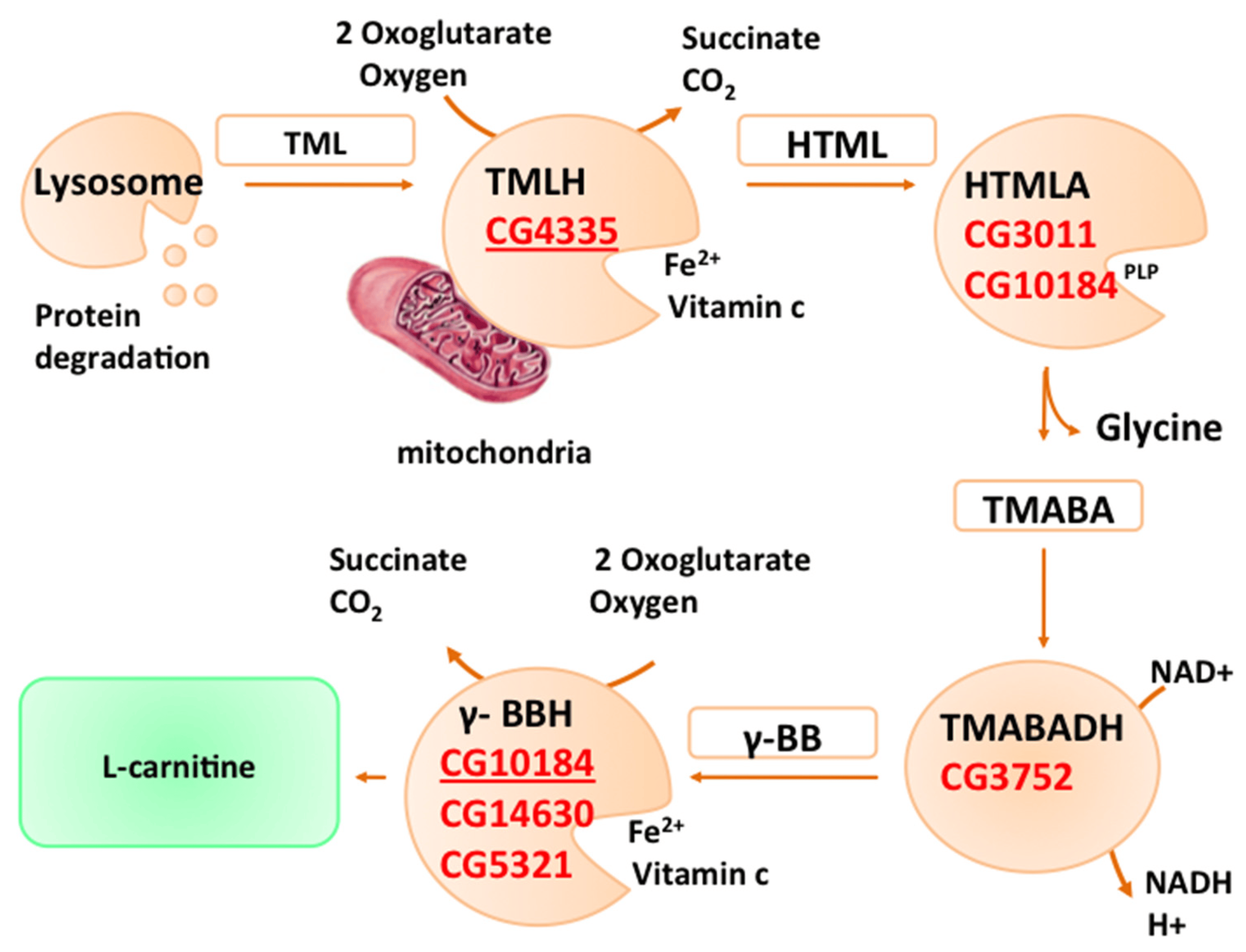
Serum carnitine refers to the concentration of carnitine, a quaternary ammonium compound, in the blood. Carnitine plays a crucial role in fatty acid metabolism by facilitating the transport of long-chain fatty acids into the mitochondria, where they can be oxidized to produce energy. Here’s some key information about serum carnitine:
- Function: Carnitine is essential for the transport of fatty acids across the inner mitochondrial membrane, where they undergo beta-oxidation to generate ATP, the body’s primary energy source. Carnitine acts as a carrier molecule, forming acylcarnitine complexes with fatty acids, which are then transported across the mitochondrial membrane.
- Sources: Carnitine is obtained from dietary sources (primarily meat and dairy products) and can also be synthesized endogenously in the liver and kidneys from the amino acids lysine and methionine. Dietary intake and endogenous synthesis contribute to the overall pool of carnitine in the body.
- Measurement: Serum carnitine levels can be measured using various laboratory methods, including spectrophotometry, enzymatic assays, and liquid chromatography-mass spectrometry (LC-MS). Serum carnitine levels are typically reported as total carnitine, which includes both free carnitine (unbound) and acylcarnitines (bound to fatty acids).
- Clinical Significance:
- Carnitine Deficiency: Deficiencies in carnitine can occur due to genetic disorders affecting carnitine transport or metabolism, as well as secondary causes such as chronic renal failure, liver disease, certain medications (e.g., valproic acid), and inadequate dietary intake. Carnitine deficiency can impair fatty acid oxidation and ATP production, leading to symptoms such as muscle weakness, fatigue, cardiomyopathy, and hypoglycemia.
- Primary Carnitine Deficiency (PCD): PCD is a rare genetic disorder characterized by impaired carnitine transport, resulting in low levels of carnitine in tissues and blood. PCD can present with symptoms such as muscle weakness, cardiomyopathy, hypoglycemia, and liver dysfunction.
- Secondary Carnitine Deficiency: Secondary carnitine deficiency can occur in conditions associated with increased carnitine excretion or decreased synthesis, such as chronic kidney disease, dialysis, certain metabolic disorders, and certain medications.
- Supplementation: Carnitine supplementation may be indicated in individuals with carnitine deficiency to correct the deficiency and alleviate associated symptoms. Supplementation can be administered orally or intravenously, depending on the severity of the deficiency and the underlying cause.
- Monitoring: Measurement of serum carnitine levels, along with clinical assessment and other laboratory tests, can help diagnose carnitine deficiency and monitor response to treatment. Monitoring may involve periodic measurement of serum carnitine levels to assess treatment efficacy and adjust supplementation as needed.
Overall, serum carnitine levels are an important parameter in the evaluation of fatty acid metabolism and the diagnosis of carnitine deficiency. Measurement of serum carnitine levels can help identify individuals at risk of deficiency and guide appropriate management strategies, including dietary modification and supplementation.

Reviews
There are no reviews yet.